One of the most frequent culprits of angst and worry for parents of children with Down syndrome is sleep. We worry they aren’t sleeping well, or long enough, or that they can’t seem to fall asleep or stay asleep. Sleep issues can affect their overall wellness, their behavior, their schooling and their mood. It certainly affects our mood as parents! In this article and the following Q&A, we hear from a pediatric sleep specialist, Dr. Thomas Stern, who talks about how we can tackle our worries and what role sleep studies and CPAP machines can play in our children’s lives. It’s not as hard as you might think! My 11-year-old son sees Dr. Stern, who diagnosed him with mild sleep apnea. He uses a CPAP successfully and its use has improved his overall stamina and energy level. – Vicki Vila, parent and volunteer blog editor
By Dr. Thomas P. Stern, MD, MS, FAASM, FCCP
Several times a month I meet a very distraught parent for the first time with the complaint “my child just doesn’t sleep.” They are always accompanied by a child that is conscious and breathing. I reply that their child must be sleeping, because if the child wasn’t sleeping at all, they would be dead within two weeks. That comment is not usually well received, but I feel it is an important point to make. I follow up that statement with a question of my own: “If I came in the room and told you that I have not been breathing the last two weeks would you believe me?” Most of the time I receive an answer like “of course not.” I then ask why and they reply, “Because you would be dead.”
Both breathing and sleep are essential human functions for life. Without them, we die. The good news is that these two functions are not optional. Humans cannot hold their breath until they die. At worst you will pass out and start breathing again. Humans cannot sleep deprive themselves until they die. You will fall asleep standing up before that happens.
(There are in fact very rare disease states that are exceptions to the above paragraph. But one is diagnosed during infancy and the other is a disease of adults. These are not relevant to patients being seen in an outpatient pediatric setting.)
There are clear differences in sleep between children with Down syndrome and children who are developmentally typical. There is a well-described association between Down syndrome and sleep apnea. The association was first described in the late 1980’s. There are several explanations for this association, including low muscle tone and consistent craniofacial features. Children with Down syndrome can also possess risk factors for sleep disordered breathing, which are not unique to the syndrome, such as tonsillar enlargement, obesity and heart disease.
Despite the increase in baseline risk for sleep apnea in children with Down syndrome, not all children with Down syndrome have it. The estimated prevalence for sleep apnea in children with Down syndrome is anywhere between 25% and 75%. This is clearly increased related to the general pediatric population, where the prevalence is around 2%. The variation for the reported prevalence is due to an absence of a standardized definition of pediatric sleep apnea.
This association between Down syndrome and sleep apnea complicates drawing conclusions between Down syndrome and other sleep abnormalities. Sleep apnea makes sleep architecture abnormal. Patients with sleep apnea experience more arousals, more movements and decreased proportions of REM sleep. Any research on sleep architecture in children with Down syndrome that does not control for sleep apnea is of limited value. Unfortunately that leaves very little data from which to draw conclusions about other co-morbid sleep disorders.
There are a few conclusions that can be drawn despite this lack of control. There are several studies to support that circadian rhythms are intact in children with Down syndrome. These studies were designed comparing children with Down syndrome to neurotypical controls. The studies used measures of movement and also hormone secretion. This suggests children with Down syndrome can have normal sleep/wake patterns when underlying sleep disorders are addressed.
I personally do not approach pediatric sleep patients with Down syndrome any differently than pediatric patients without it, with the exception of having a high index of suspicion of sleep apnea. Once sleep apnea is ruled out, my approach to a pediatric patient with Down syndrome is the same as my approach to a neurotypical pediatric patient regardless of the complaint. Other sleep disorders such as narcolepsy, sleep related seizures, or a movement disorder such as parasomnia or restless legs syndrome need to be considered.
While neuropsychiatric disorders such as autism, anxiety, post traumatic stress disorder, etc. will have sleep manifestations, they are not considered primary sleep disorders and treatment should focus on the underlying disorder. Unfortunately, pharmacologic treatments for these disorders often have adverse effects on sleep. Psychiatric medications can be sedating and thus cause sleepiness, or stimulating, thus preventing sleep. If your child is on a medication that affects sleep, you are stuck between a rock and a hard spot. You will have to work with the healthcare provider to find a balance between effect and side effect.
Parents seem to put all of their focus on when children go to sleep. If children don’t go to sleep on command, they conclude there is a problem. If a child does not go to sleep when the parent wants, it creates anxiety for the parent and this is often communicated to the child. The parent gets upset, the child gets upset and no one sleeps. There are a few things in life you cannot force your child to do. One of them is sleep. If you try and force your child to sleep, you are guaranteeing yourself failure.
Sleep Tip #1: Do not focus on when your child sleeps. Focus on when they stay awake. The longer a human is awake, the more likely they are to fall asleep and stay asleep. It is just how the brain works. If you do not feel your child is sleeping well at night, do not let them sleep during the day. Conversely, if your child must sleep during the day, make their bedtime later. It is abnormal for school-aged children, about age 5 and up, to nap during the day. In fact if they need to nap, they are either sleep deprived or they have a sleep disorder. Recommended sleep times vary by age and can be found here: (https://www.sleepfoundation.org/press-release/national-sleep-foundation-recommends-new-sleep-times). If a child wakes at night, either their sleep drive is not being optimized or their sleep is being disrupted. Sleep disruption can be caused by medications, environmental factors and sleep disorders.
The human brain is designed to sleep at night and be awake during the day. It is very influenced by light. While you cannot control the sun and the moon, most households have direct light sources that influence sleep. Direct light sources are lights that you look into such as televisions, computers and cell phones. Tip #2: Do not let your child use a direct light source within 90 minutes of bedtime. Using a direct light source within 90 minutes of bed can delay sleep onset. Teenagers seem to be the most susceptible. Likewise, if you want to promote an earlier bedtime, expose your child to a bright light (sunlight is the best) soon after they wake up.
The third major sleep promoter is the amount of physical activity your child has during the preceding wake period. Tip #3: Keep your child as physically active during the day as possible. Studies have shown the more “screen time” children have during the day, the poorer their sleep quality is. Physical activity is best earlier in the day. I would discourage intense physical activity within 2 hours of bedtime, but plenty of children that are physically active all day can get in bed and fall asleep soon after.
If a child that stays awake all day, is physically active during the day, avoids sleep preventers (medicines, lights, noise, etc.,) and is unable to sleep, then it would be a good idea to see a pediatric sleep specialist.
Dr. Stern practices at Advanced Respiratory and Sleep Medicine, with offices in Huntersville and Hickory, NC. He completed a residency in internal medicine and pediatrics and fellowships in pulmonary medicine, critical care medicine and sleep medicine. His pediatric sleep medicine training was at Rainbow Babies and Children’s Hospital in Cleveland, OH.
Ask the Sleep Doctor: Some of Parents’ Most Frequently Asked Questions
1) Is it still recommended for a child with Down syndrome to do a sleep study even if they don’t exhibit specific concerns? At what age?
Yes – it is recommended that all children with Down syndrome get a sleep study by 4 years of age. Children should have the study with or without symptoms because children with Trisomy 21 may not have traditional symptoms.
2) What would be considered concerning symptoms?
Snoring, restless sleep, waking unrefreshed, frequent or early arousals.
3) What can the short- and long-term effects of untreated apnea be?
Short-term effects are manifestations of sleep deprivation including irritability, inattention, and hyperactivity. Longer-term effects are growth retardation and cardiovascular complications.
4) A few parents said they’ve had multiple sleep studies done and results were inconclusive. The parents report they feel their child DOES have sleep issues and they wonder if there are other ways to get sleep data besides a sleep study if those are inconclusive.
I highly recommend patients only be studied in a place with people formally trained in pediatric sleep. There is a significant difference in performing and interpreting pediatric studies and adult studies. People not trained in pediatric sleep don’t understand this. The only way a sleep study would be inconclusive is if the child does not sleep. It is important keep the child awake and active the day before the study so they will sleep. There is no other way to get good data on children other than a traditional sleep study.
5) Some parents report that their children cannot do sleep studies because the child flops around too much, the wires or nasal cannula keep coming off and they simply can’t sleep, so technicians end their studies without data. What would you advise a parent whose child struggles with the studies? Some have asked if it is all right to sedate children for a sleep study?
I would never recommend a study that involves sedating children. If the child sleeps and they are at a good pediatric center, there will not be inconclusive data. A nasal cannula is not necessary to do a sleep study. There are options that are better tolerated than the nasal cannula — such as thermistors and RIP-sum belts.
6) Some parents wonder if it’s worth doing a sleep study if they’ve already had their child’s tonsils and adenoids out, and they feel that their child won’t tolerate a CPAP. Are there other “end results” or recommendations that can come out of a sleep study besides CPAP?
There are other options for treating sleep apnea in children. Maxillary expansion with orthodontia can be very helpful. Treating nasal congestion with medicine can also be helpful. Restless legs or hyperactivity is traditionally a clinical diagnosis that should lead to a ferritin level check. It certainly can manifest on a sleep study.
CPAP, though, is currently the only treatment for apnea that is guaranteed to work and is covered by insurance.
Parents have different levels of effectiveness with children, whether it is CPAP or eating vegetables. In order to implement PAP, you must have parents that are willing to be insistent and persistent. The kids will wear it.
7) So what CAN parents do if their child is not tolerating the CPAP?
Optimizing the CPAP setup – in terms of settings and mask – is important. Most medical equipment companies have no idea what they are doing with adults, let alone children, so it is important to work with the pediatric sleep physician to troubleshoot. Patience and persistence is key.
The initial goal should be brief nightly exposure. Get the child to put it on every night for a few minutes. Reward them if they keep it on 15min, 30 min, etc. Then make the reward if they fall asleep with it on. Teaching them to fall asleep with it on is the main hurdle. Once they can do that, they will usually wear it for several hours. It is not important that they wear it 100% of the time.
When you go to follow up appointments with your sleep doctor, they will look at the compliance and efficacy data from your machine to see how long your child has kept the mask on each night. Good compliance is considered an average of at least 4 hours on most nights.
Once your child is able to fall asleep with the mask on, check and readjust before you go to bed yourself, but you do not feel the need to get up in the middle of the night to put it back on.
8) Going along with this, what are the other, newer options they can explore after they’ve given CPAP a good try? There is a procedure called the hypoglossal nerve stimulator, for example, that is being studied in adults. Some parents ask if prescription medications could be given along with the mask to help their child sleep better.
Nerve stimulators are much less effective in adults than CPAP. It involves a surgery and there are significant side effects. There are no clinical trials in children — only case series. I would not recommend in a child until there is more data. I would never sedate a child to wear PAP. If the set up is reasonable, children will wear it with insistence and persistence. I have seen a lot of crazy setups in patients that come from labs that don’t know how to treat children. If they have not seen a pediatric sleep expert, they have not failed yet.
9) Can a child with Down syndrome be given melatonin to help promote sleep? If so, how would parents know the correct dosage?
As I mentioned previously, research suggests that circadian functions are intact in patients with Down syndrome. The only one that specifically looked at 24-hour melatonin levels showed no difference in mean levels when compared to neurotypical controls (https://www.ncbi.nlm.nih.gov/pubmed/8648562) so melatonin supplementation should not be necessary. I do not think melatonin will hurt though. When using melatonin, it is important to give it at the same time every night in conjunction with a good sleep/wake schedule. Consult your pediatrician to discuss a starting dosage.
10) We have some in our population with very severe, even life-threatening apnea, including adults with Down syndrome. Do you have any advice for this population?
The difference between the child and the adult is that you usually have to deal with the adult in a direct manner. This is tough.
Again, #1 is optimizing set up. I wear CPAP every night and routinely see adult patients with setups I could not wear. Using auto-titrating machines is important because it allows people to start with very low pressures. Auto-titrating machines are more expensive to the medical equipment company so people will hesitate to prescribe them. Letting the patient choose the mask is also very important. Too often patients are give masks that optimize profit rather than provide comfort.
Finally, getting the patient to believe in the need for PAP is absolute. If an adult does not want to wear PAP (or comply with any other therapy) they won’t.
Try modeling yourself wearing a mask before bed. Be succinct and encouraging.
“I know wearing CPAP is hard, but it is very important for you health. You can do this. We want you to be healthier and feel better.”
Patients with Down syndrome and caregivers of patients with Down syndrome are faced with a lifetime of unique health challenges that can be very serious and stressful. Dealing with sleep disorders is very rarely serious and should not be stressful. The first step is to partner with healthcare providers who are trained in and comfortable with addressing the issues you are struggling with. It is also important to understand that there are no “magic pills” and dealing with sleep problems will require patience and persistence from the patient, the caregiver and the healthcare provider. – Dr. Thomas P. Stern
 David and Lisa Cooper get to work alongside their adult son, Zach, each day as they make doughnuts, cinnamon rolls, apple fritters, and other sweet delights at Down for Doughnutsin Mooresville, NC, which is north of Charlotte. Zach has Down syndrome and families like the Coopers understand the difficulties of finding employment for those with disabilities. In fact, a comprehensive study commissioned by Special Olympics found, “unemployment among people with intellectual disabilities is more than twice as high as for the general population.”
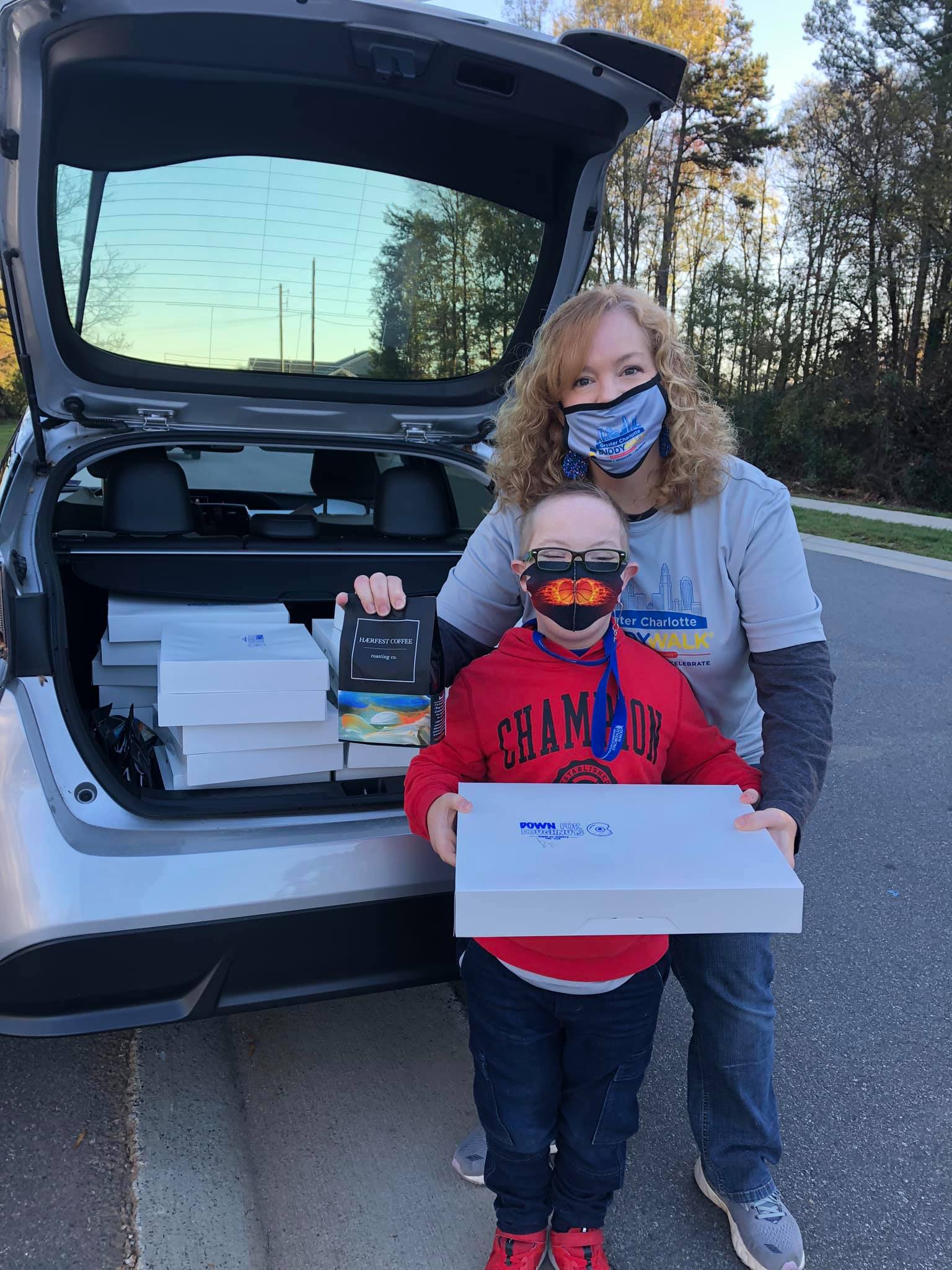
David and Lisa Cooper get to work alongside their adult son, Zach, each day as they make doughnuts, cinnamon rolls, apple fritters, and other sweet delights at Down for Doughnutsin Mooresville, NC, which is north of Charlotte. Zach has Down syndrome and families like the Coopers understand the difficulties of finding employment for those with disabilities. In fact, a comprehensive study commissioned by Special Olympics found, “unemployment among people with intellectual disabilities is more than twice as high as for the general population.” Charlotte (NC) teenager Reid Foreman is learning the family coffee roasting business at HÆRFEST COFFEE (pronounced “harvest”). His dad, Toby, is a former Major League Baseball pitcher who fell in love with the coffee industry years ago while recovering from elbow surgery. When Toby’s wife, Cheri, gave birth to Reid and received his Down syndrome diagnosis, they promised each other to move forward on HÆRFEST COFFEE because, “Reid and his friends will need jobs someday,” recalls Toby.
Charlotte (NC) teenager Reid Foreman is learning the family coffee roasting business at HÆRFEST COFFEE (pronounced “harvest”). His dad, Toby, is a former Major League Baseball pitcher who fell in love with the coffee industry years ago while recovering from elbow surgery. When Toby’s wife, Cheri, gave birth to Reid and received his Down syndrome diagnosis, they promised each other to move forward on HÆRFEST COFFEE because, “Reid and his friends will need jobs someday,” recalls Toby. the size and quantity you need, right on time to remind each you to change the dirty ones in your home. Kennedy has a twin brother, Jacob, who does not have Down syndrome, and their parents want to make a future where both will have similar opportunities to thrive. “We’re changing the systems so that Kennedy and Jacob can both benefit from a quality education, live independently as adults, pursue meaningful work, and contribute to their chosen communities and neighborhoods with our nonprofit KennedyStrong, which receives a portion of each purchase from The Filter Box.”
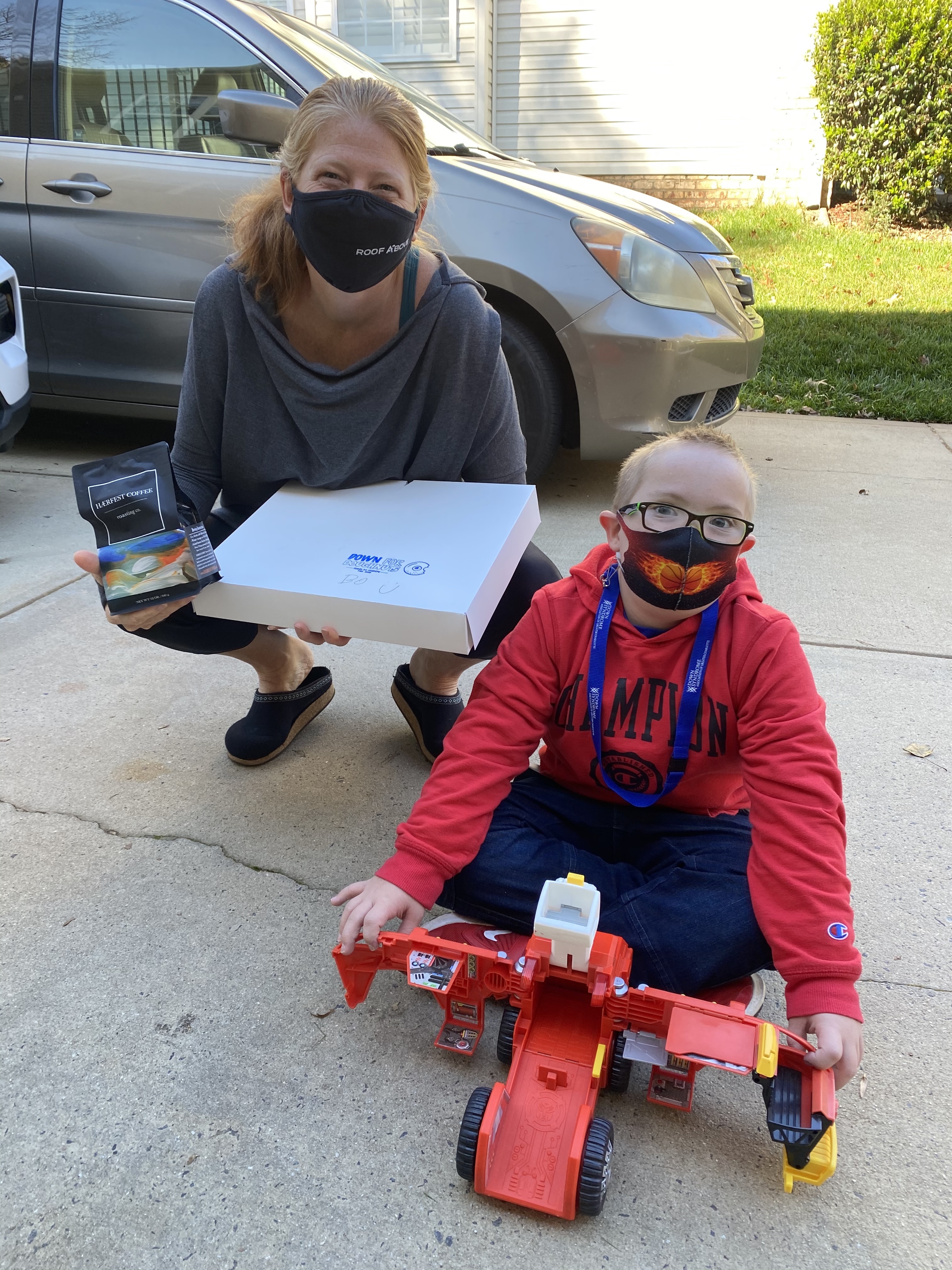
the size and quantity you need, right on time to remind each you to change the dirty ones in your home. Kennedy has a twin brother, Jacob, who does not have Down syndrome, and their parents want to make a future where both will have similar opportunities to thrive. “We’re changing the systems so that Kennedy and Jacob can both benefit from a quality education, live independently as adults, pursue meaningful work, and contribute to their chosen communities and neighborhoods with our nonprofit KennedyStrong, which receives a portion of each purchase from The Filter Box.” The “Sweet Spot Package” is 1-dozen glazed doughnuts delivered to your business or home for $25, while the “Better Together Package” is 1-dozen glazed doughnuts plus a 12 oz. bag of whole bean coffee delivered to your home or business for $40. Lisa Ciaravella, a Realtor with Kindred Realty, bought packages for delivery as a corporate “thank you gift” to nine of her clients who closed on new homes this year. “We wanted to give our clients a unique gift they’d enjoy, that supports people with disabilities, which is an effort close to our hearts,” says Lisa, whose family also owns Phoenix Physical Therapy and Sports Performance which helps patients with physical disabilities.
The “Sweet Spot Package” is 1-dozen glazed doughnuts delivered to your business or home for $25, while the “Better Together Package” is 1-dozen glazed doughnuts plus a 12 oz. bag of whole bean coffee delivered to your home or business for $40. Lisa Ciaravella, a Realtor with Kindred Realty, bought packages for delivery as a corporate “thank you gift” to nine of her clients who closed on new homes this year. “We wanted to give our clients a unique gift they’d enjoy, that supports people with disabilities, which is an effort close to our hearts,” says Lisa, whose family also owns Phoenix Physical Therapy and Sports Performance which helps patients with physical disabilities. There are still openings for doughnut and coffee deliveries this December 18 and 19, the last two dates of this pop-up fundraiser. Brodie’s mom, Kathy Rummage, who’s the driver for her young delivery guy, says the smiles they’ve collected at each stop along the way, are well worth the miles. But she’s most optimistic about the gift that didn’t come inside a box or bag.“One of the goals of Donate for Doughnuts is to bring people with Down syndrome to the greater community, to people who haven’t had the chance to meet, talk, and laugh with someone who’s differently abled,” she says. “It’s vitally important our kids have better exposure in their neighborhoods, towns, and schools so their neighbors and peers will be able to recognize their ability first. What a better way to create those relationships than over doughnuts and coffee!”
There are still openings for doughnut and coffee deliveries this December 18 and 19, the last two dates of this pop-up fundraiser. Brodie’s mom, Kathy Rummage, who’s the driver for her young delivery guy, says the smiles they’ve collected at each stop along the way, are well worth the miles. But she’s most optimistic about the gift that didn’t come inside a box or bag.“One of the goals of Donate for Doughnuts is to bring people with Down syndrome to the greater community, to people who haven’t had the chance to meet, talk, and laugh with someone who’s differently abled,” she says. “It’s vitally important our kids have better exposure in their neighborhoods, towns, and schools so their neighbors and peers will be able to recognize their ability first. What a better way to create those relationships than over doughnuts and coffee!”



 e an actor.
e an actor. 
 and clever, especially when he escapes the nursing home and also throwing his nursing friend’s car keys in the ocean. That was funny. Just like me, he knows what he likes and wants.” With Zak’s humor, intelligence, and kindness he changes the hard and tough Tyler for the better. Rea also said that when Tyler and Zak become friends, Tyler “sees that it doesn’t matter if somebody has Down syndrome, he is just a regular person.” Rea hits it on the nose there. All people have different abilities and skills that can enhance both their own life and the lives of others. As Maners said, “Zak doesn’t wait to love.” Maners sees this same loving quality in her 10-year-old son, Branson, “everyone is his new best friend.” Zak loves Tyler without judgment of his past mistakes.
and clever, especially when he escapes the nursing home and also throwing his nursing friend’s car keys in the ocean. That was funny. Just like me, he knows what he likes and wants.” With Zak’s humor, intelligence, and kindness he changes the hard and tough Tyler for the better. Rea also said that when Tyler and Zak become friends, Tyler “sees that it doesn’t matter if somebody has Down syndrome, he is just a regular person.” Rea hits it on the nose there. All people have different abilities and skills that can enhance both their own life and the lives of others. As Maners said, “Zak doesn’t wait to love.” Maners sees this same loving quality in her 10-year-old son, Branson, “everyone is his new best friend.” Zak loves Tyler without judgment of his past mistakes.