We had the privilege of hosting three remarkable guests on WCNC’s Charlotte Today program. They discussed Down Syndrome Awareness Month and our upcoming Buddy Walk. Whenever the opportunity arises, we are always eager to educate the community about Down syndrome.
Thank you to Brooke Fields Christenburg, Lincoln, and Cody for representing the Down Syndrome community.
If you have lived with someone with Down syndrome you know that it is a MYTH that they are always happy. Individuals with Down syndrome experience a variety of emotions and may demonstrate symptoms and behaviors related to depression, anxiety, and other mental health diagnoses.
Everyone with Down syndrome is a unique individual but there are common characteristics often seen across the Down syndrome population. Some of these characteristics and their potential impact on mental health are listed below:
Perceptive of Others’ Emotions: I have had several families tell me that their loved one has a “6th sense” when it comes to detecting others’ stress and always seem to know when someone needs comforting. This highly perceptive nature can also negatively impact individuals with Down syndrome. If anyone else in your home is struggling with their mental health, sometimes family members with Down syndrome will mimic others’ behaviors and emotions and appear stressed or depressed themselves.
Prefer Sameness: Dr. Chicoine and Dr. McGuire use the term “the groove” in their book, Mental Wellness in Adults with Down Syndrome, 2nd Edition, to describe routines that individuals with Down syndrome often use to function. The routines can promote independence; however, if the routine has become too rigid or they have gotten stuck in a negative routine, it may be more difficult and take more time to transition back to healthy living habits.
Difficulty Recognizing Passage of Time: When remembering a negative event, for example, a death, your family member might experience strong emotions like the event that occurred yesterday as opposed to several years ago. Sometimes just the mention of a similar negative event in someone else’s life will elicit these strong emotions as well.
Strong Long-term Memory: Although this is often viewed as a strength, when it comes to traumatic events, being able to recall every detail of the event may in fact make it more difficult for your family member to move through the grief process.
Self-Talk: Many individuals with Ds talk to themselves in a way that is audible to others. This behavior is often used to process feelings and plan out their day. If the language and/or tone changes and becomes angry or they seem “stuck” in the conversation, it may indicate that they are experiencing pain, stress, or are bothered in some way.
Medical Conditions: It is important to have a medical exam prior to or in addition to receiving mental health treatment. Physical illnesses can present as behavior changes or as mental health symptoms. Sleep disturbances, thyroid or gastrointestinal issues are often seen in individuals with Down syndrome and may present as irritable, depressed, anxious or lethargic behaviors.
Did any of the above sound familiar? If so, you may find comfort in the fact that most of the behaviors are typical of individuals with Down syndrome and intervention is not always necessary. If you decide to seek counseling, it is important that you find a clinician that is familiar with Down syndrome so that your family member is not misdiagnosed or over-prescribed.
In working with clients with Down syndrome, I have observed the importance of treating the whole individual. Mental health, physical health, healthy relationships, and meaningful opportunities all work together to promote a healthy and happy life. Listed below are skills and focus areas that I often address in counseling with my clients. I have provided examples of activities to assist your family member in developing these skills. Please note, this list is meant to provide ideas for self-help and should not be used as a substitute for therapy or mental health care.
Focus on the Whole Person- Mental Health Target Areas Include:
1. Cognition– Dr. Brian Skotko has a “Brain Train Video Series” where he discusses ways to boost cognition. Some of his recommendations include open-ended questions in short 5-minute conversations, brain exercises to include activities like word searches and matching games, and of course healthy eating, physical activity, and socialization…more on those later!
2. Self-advocacy– Strong self-advocacy skills often increase confidence. Talk to your loved one about their goals. Have discussions and help them identify their strengths, struggles, likes and dislikes. Normalize asking for help and role-play appropriate ways to do this. Let them know that it is always ok to speak up for themselves if something is happening that is making them uncomfortable. Practice problem-solving and conflict resolution using “what if” scenarios.
3. Psychoeducation– Many of my clients have been empowered after simply learning about their diagnosis and its related symptoms. Provide education about mental health, why it is important, and what factors in our lives work together to keep us healthy and happy. It is also helpful to teach healthy living habits in general and how exercising our minds, keeping our bodies active, maintaining an organized environment, and focusing on others can bring us joy.
4. Emotional literacy– This area focuses on increasing one’s ability to express emotions. Have your family member practice using feelings words. Provide them with a list of these words or a visual showing facial expressions related to various emotions. Individuals with Down syndrome are often visual learners, help them learn more about their own emotions by identifying the feelings of others in movies, on tv, and out in the community. You can also use mainstream games to increase discussions around emotions. In UNO or Candyland, depending on what color you land on, discuss a different emotion. (Ex. Red- tell me about a time you felt angry. What did you do to make yourself feel better? Blue- a time you felt sad. Yellow- what makes you happy.) Use JENGA blocks as conversation starters by writing questions on the blocks. Each time the player removes a block they must answer a question or discuss what is on the block.
5. Coping skills– A few common calm-down techniques are listed below. It is recommended that you introduce these activities when your family member is calm, not after they have already become upset. Try practicing these skills at bedtime…maybe the exercise will help them sleep! I suggest putting together a coping skills folder of visual aids… no matter the family member’s age or abilities. In a time of frustration, minimal conversation is best. Simply reference the calm-down folder as a reminder to use these tools. Resources for visuals are listed below.
Deep breathing– teach your family member to breathe in through their nose like they are smelling a flower and blow out through their mouth, like blowing out birthday candles.
Muscle relaxation– squeezing a stress ball or giving yourself a big hug. The key is recognizing the difference between when your body is tense versus relaxed.
Grounding– we often stress over things that happened in the past or are coming up in the future. Grounding helps us focus on the present and our current surroundings. Practice the 5-4-3-2-1 method: look around and identify 5 things you can see, touch 4 things, identify 3 things you can hear, notice 2 things you smell, and say 1 positive thing to yourself.
Gratitude Practice– make a list of 3 things, people, places, or activities that bring you joy. The list can be written, texted in the notes of a phone, or voice recorded to modify the exercise.
6. Relationships, Boundaries & Sexuality Education– this could be a separate blog post of its own! I have found that many of my clients initiate counseling due to some sort of relationship/social issue. Because of this, I include relationships, boundaries, safety and communication lessons as part of the counseling process. Struggles that I have encountered frequently and brief descriptions of what I try to do to help are listed below.
Isolation– assists in connecting with the community.
Few meaningful relationships– identify characteristics of healthy and unhealthy relationships and assist in developing friendship skills.·
Misunderstanding boundaries with coworkers and peers– Circles Curriculum and PEERS role-play practice.
Desire to have a sweetheart– talk to them about how relationships develop – everything from having a crush, flirting, dating, healthy vs unhealthy behaviors, communication, and breaking up.
Internet safety– only converse with friends and family you have met in real life. Never give anyone money or personal information over the Internet. Celebrities will not ask to chat with you privately.
Increased risk of sexual abuse– sex education is about understanding consent, the right to say no, appropriate names for private parts, sexual acts, and safety planning.
7. Community Connections– if my clients are at home with little to no peer interactions or involvement in meaningful activities, they will still be depressed. Counseling and medication can go so far, but I often enlist the family’s help in connecting my clients with programs, activities, and peers.
As Chris Nikic (1st person with Down syndrome to complete an IRONMAN) would say, set a goal to get “1% Better Each Day.” Make small changes in routines, implement one activity at a time, and do not feel pressured to introduce all target areas at once. Remember, it is never too early or too late to address these skills… lifelong learning is key!

References & Resources:
Dr. Skotko video series- https://www.downsyndromebraintrain.com/products
Mental Wellness in Adults with Down Syndrome, 2nd Edition. Free PDF- https://adscresources.advocatehealth.com/mental-wellness-in-adults-with-down-syndrome-2nd-edition/
Adult Down Syndrome Center Resource Page-https://adscresources.advocatehealth.com/search/people-with-down-syndrome
DSCBA Mental Health Padlet- https://padlet.com/DSCBA/dscba-mental-health-alliance-ottzudfzmka3q8n7
YouTube mindfulness videos-https://www.youtube.com/results?search_query=mindfulness+videos+for+teens
Circles Curriculum- https://stanfield.com/product/circles-curriculum-bundle-w1004-38/
PEERS Role Play Videos- https://www.semel.ucla.edu/peers/resources/role-play-videos
Relationship & Sexuality Education- www.amaze.org
No Limits Counseling Website: www.nolimitscounseling.org
Michele Mattox, LCSW, LISW-CP.
Michele is a Licensed Clinical Social Worker in North and South Carolina. She founded No Limits Counseling & Coaching, a private practice that was developed specifically for teens and adults with I/DD. She provides virtual mental health counseling to individuals with Down syndrome throughout NC and SC. Michele also offers relationship coaching in the form of groups by partnering with disability organizations. Group topics include: Relationships, boundaries, friendship, dating, and sexuality.
Michele is closely connected to the Down syndrome community and spent many years volunteering at various non-profits in the Charlotte area. It was during this time that she realized the need for more mental health professionals that are familiar with and can connect with individuals with Down syndrome. Michele’s experience in the disability community over the last 20 years has given her insight into mental health and relationship struggles often experienced by individuals with Down syndrome.





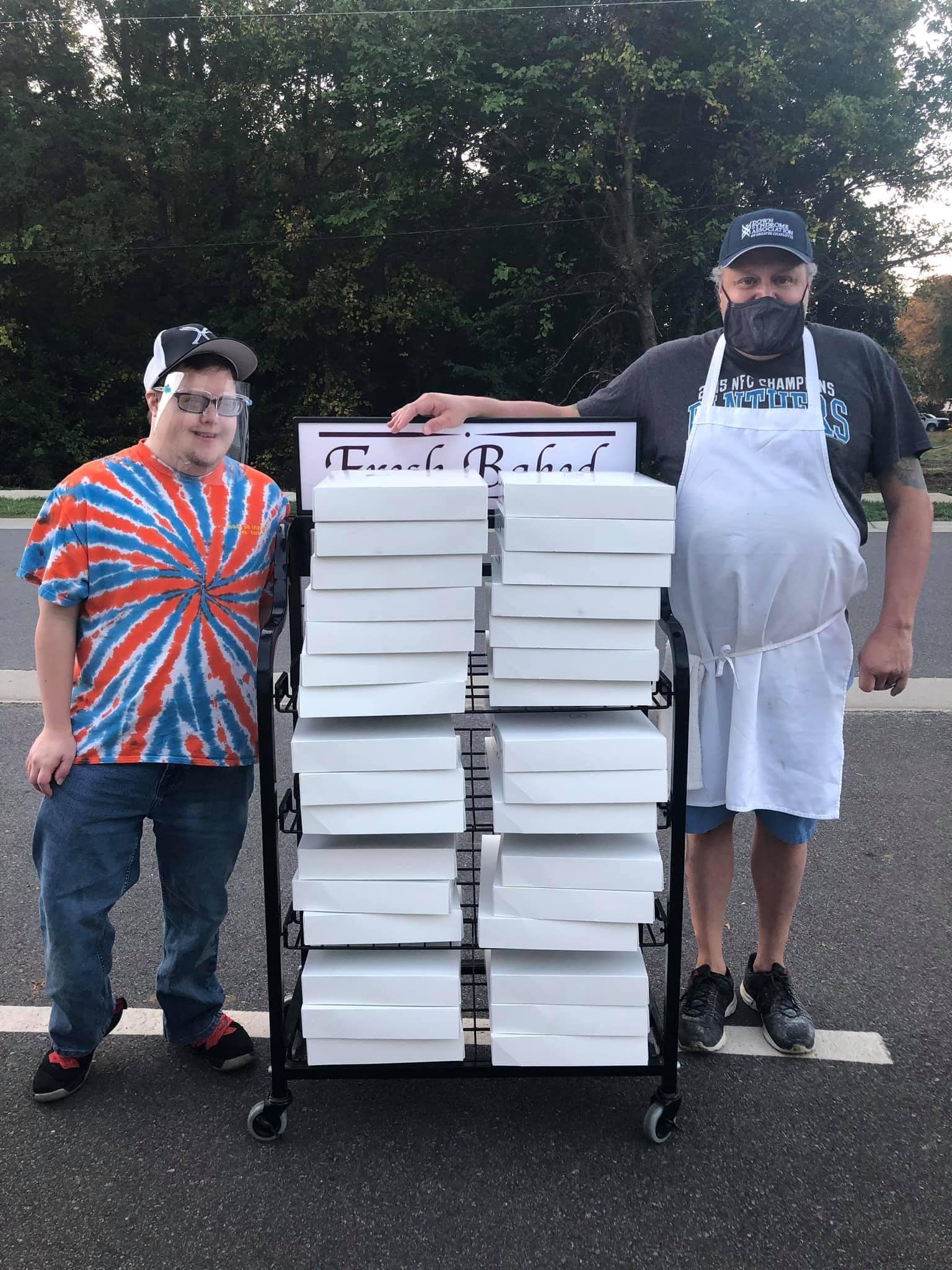 David and Lisa Cooper get to work alongside their adult son, Zach, each day as they make doughnuts, cinnamon rolls, apple fritters, and other sweet delights at
David and Lisa Cooper get to work alongside their adult son, Zach, each day as they make doughnuts, cinnamon rolls, apple fritters, and other sweet delights at  Charlotte (NC) teenager Reid Foreman is learning the family coffee roasting business at
Charlotte (NC) teenager Reid Foreman is learning the family coffee roasting business at  the size and quantity you need, right on time to remind each you to change the dirty ones in your home. Kennedy has a twin brother, Jacob, who does not have Down syndrome, and their parents want to make a future where both will have similar opportunities to thrive. “We’re changing the systems so that Kennedy and Jacob can both benefit from a quality education, live independently as adults, pursue meaningful work, and contribute to their chosen communities and neighborhoods with our nonprofit
the size and quantity you need, right on time to remind each you to change the dirty ones in your home. Kennedy has a twin brother, Jacob, who does not have Down syndrome, and their parents want to make a future where both will have similar opportunities to thrive. “We’re changing the systems so that Kennedy and Jacob can both benefit from a quality education, live independently as adults, pursue meaningful work, and contribute to their chosen communities and neighborhoods with our nonprofit  The “Sweet Spot Package” is 1-dozen glazed doughnuts delivered to your business or home for $25, while the “Better Together Package” is 1-dozen glazed doughnuts plus a 12 oz. bag of whole bean coffee delivered to your home or business for $40.
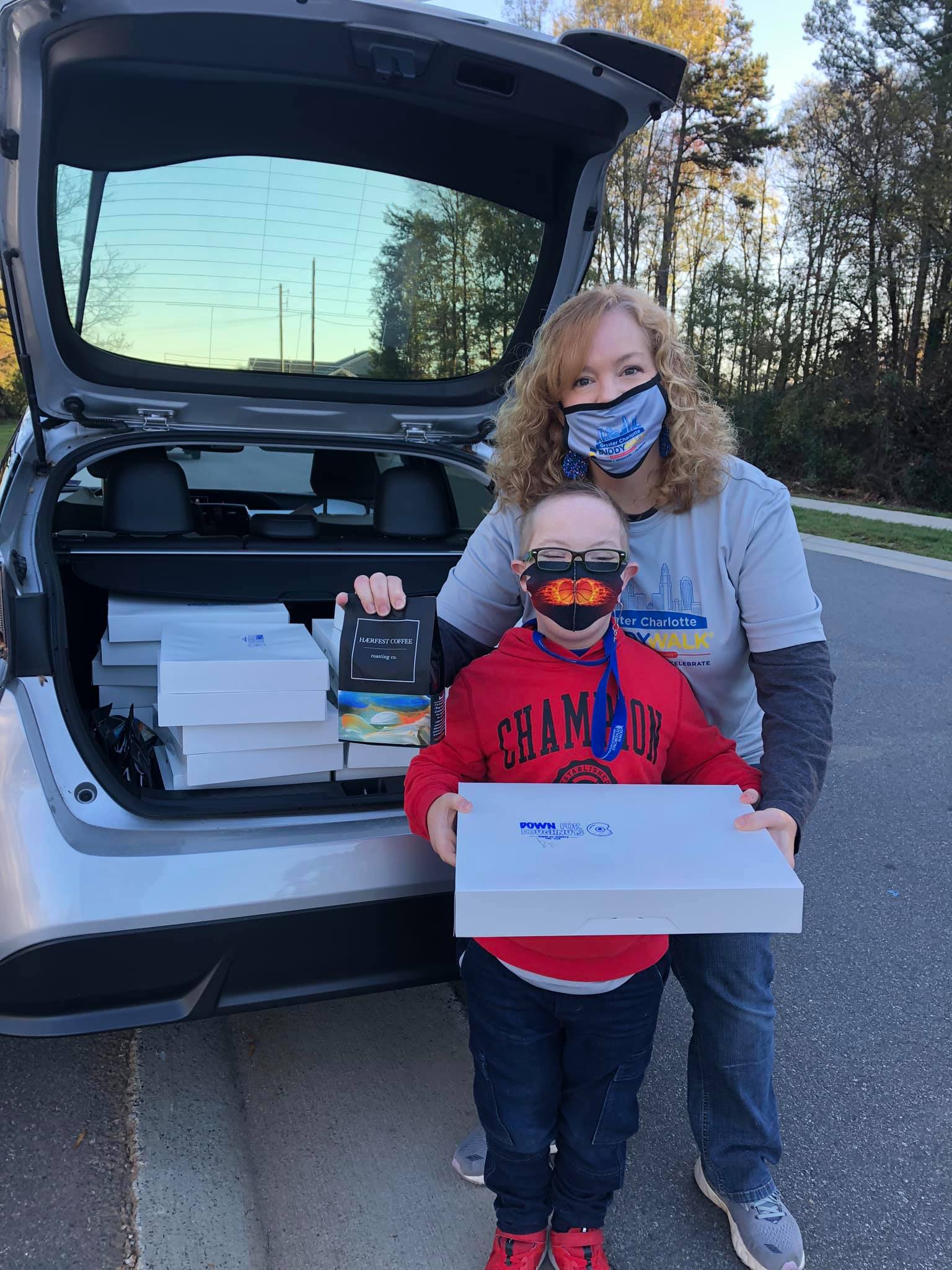
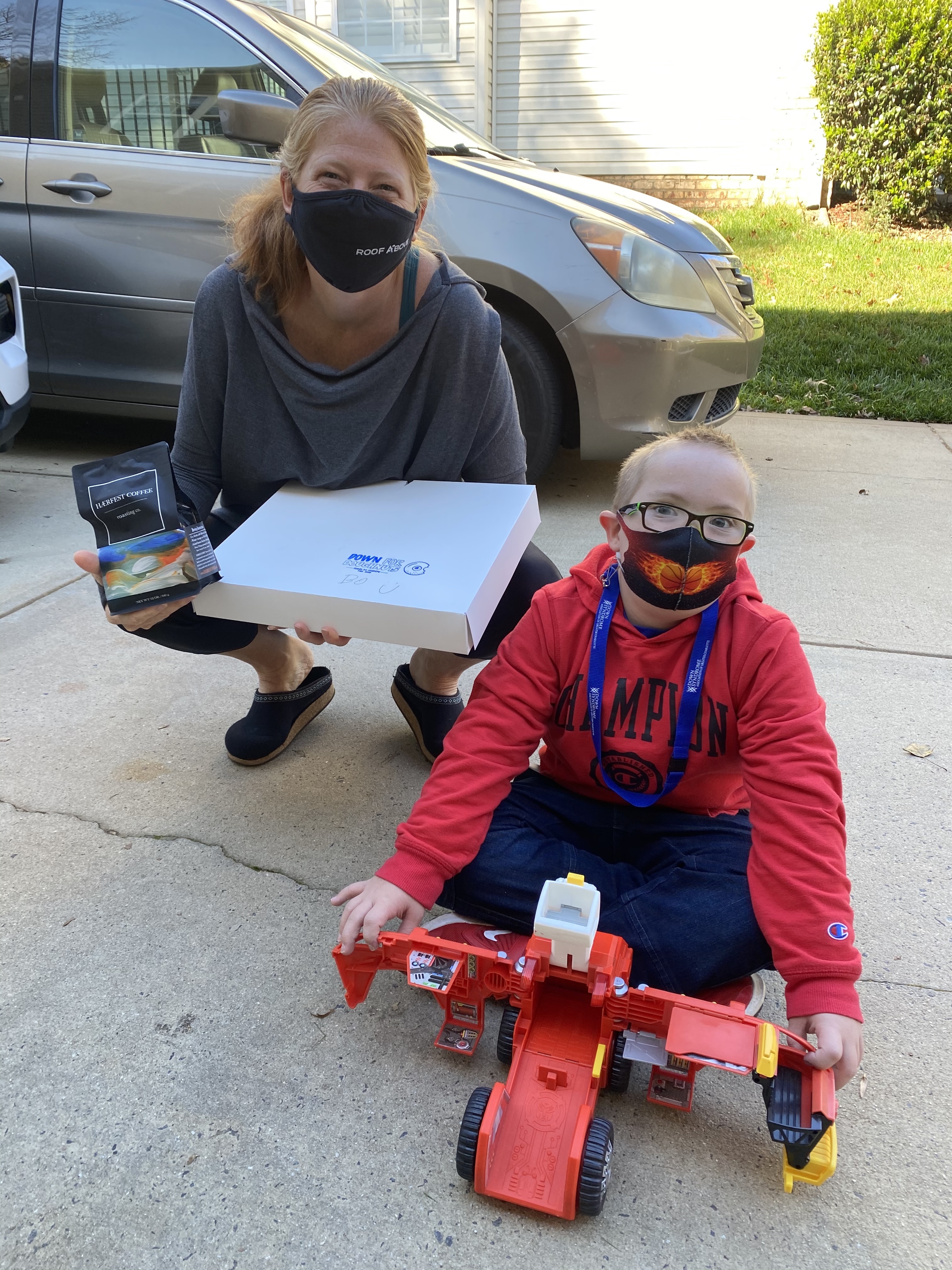
The “Sweet Spot Package” is 1-dozen glazed doughnuts delivered to your business or home for $25, while the “Better Together Package” is 1-dozen glazed doughnuts plus a 12 oz. bag of whole bean coffee delivered to your home or business for $40.  There are still openings for doughnut and coffee deliveries this December 18 and 19, the last two dates of this pop-up fundraiser. Brodie’s mom, Kathy Rummage, who’s the driver for her young delivery guy, says the smiles they’ve collected at each stop along the way, are well worth the miles. But she’s most optimistic about the gift that didn’t come inside a box or bag.“One of the goals of Donate for Doughnuts is to bring people with Down syndrome to the greater community, to people who haven’t had the chance to meet, talk, and laugh with someone who’s differently abled,” she says. “It’s vitally important our kids have better exposure in their neighborhoods, towns, and schools so their neighbors and peers will be able to recognize their ability first. What a better way to create those relationships than over doughnuts and coffee!”
There are still openings for doughnut and coffee deliveries this December 18 and 19, the last two dates of this pop-up fundraiser. Brodie’s mom, Kathy Rummage, who’s the driver for her young delivery guy, says the smiles they’ve collected at each stop along the way, are well worth the miles. But she’s most optimistic about the gift that didn’t come inside a box or bag.“One of the goals of Donate for Doughnuts is to bring people with Down syndrome to the greater community, to people who haven’t had the chance to meet, talk, and laugh with someone who’s differently abled,” she says. “It’s vitally important our kids have better exposure in their neighborhoods, towns, and schools so their neighbors and peers will be able to recognize their ability first. What a better way to create those relationships than over doughnuts and coffee!”


 e an actor.
e an actor. 
 and clever, especially when he escapes the nursing home and also throwing his nursing friend’s car keys in the ocean. That was funny. Just like me, he knows what he likes and wants.” With Zak’s humor, intelligence, and kindness he changes the hard and tough Tyler for the better. Rea also said that when Tyler and Zak become friends, Tyler “sees that it doesn’t matter if somebody has Down syndrome, he is just a regular person.” Rea hits it on the nose there. All people have different abilities and skills that can enhance both their own life and the lives of others. As Maners said, “Zak doesn’t wait to love.” Maners sees this same loving quality in her 10-year-old son, Branson, “everyone is his new best friend.” Zak loves Tyler without judgment of his past mistakes.
and clever, especially when he escapes the nursing home and also throwing his nursing friend’s car keys in the ocean. That was funny. Just like me, he knows what he likes and wants.” With Zak’s humor, intelligence, and kindness he changes the hard and tough Tyler for the better. Rea also said that when Tyler and Zak become friends, Tyler “sees that it doesn’t matter if somebody has Down syndrome, he is just a regular person.” Rea hits it on the nose there. All people have different abilities and skills that can enhance both their own life and the lives of others. As Maners said, “Zak doesn’t wait to love.” Maners sees this same loving quality in her 10-year-old son, Branson, “everyone is his new best friend.” Zak loves Tyler without judgment of his past mistakes.